Understanding the Causes of Carotid Endarterectomy
Carotid artery disorder is a circumstance as a consequence of narrowing of the carotid arteries with the aid of plaque fatty materials within the arteries. This condition is called atherosclerosis, which is the main cause of carotid artery disease, and thus opportunity the likelihood of developing seizures is generally increased. Knowledge of these factors can help prevent or, if it reaches an infection stage, improve disease management.
1. High Blood Pressure (Hypertension)
Another significant risk factor that has been established to have strong links with carotid artery disease is high blood pressure or hypertension. When blood pressure is high for a shorter period, it is not a major problem, but when it is high most of the time it weakens the walls of the arteries. Constant stress puts a lot of pressure on the blood vessels reducing its ability to resist pressure thus leading to the damage and inflammation of arteries that enables the development of plaques in the process.
Therefore, the optimum ways of controlling blood pressure risks are through diet modification, increased physical activity, and medication to prevent the occurrence of carotid artery disease. Individuals can manage high blood pressure by treating it regularly, keeping their regular appointments, and following their prescribed treatments. Regular monitoring and timely intervention can significantly reduce the likelihood of requiring carotid endarterectomy due to advanced arterial damage caused by prolonged hypertension.
2. High Cholesterol
Cholesterol is one of the fats, which in its transport in the arterial blood, in turn, turns into a hard material of a cork type. Cholesterol in the blood is classified into low density-lipoprotein (LDL), commonly referred to as the “bad” cholesterol, and high density lipoprotein (HDL), called the “good” LDL cholesterol. High LDL cholesterol has a tendency to deposit cholestrolons within the carotid arteries, while excessive density lipoprotein or HDL cholesterol tends to clean it.
Therefore, reduction of the intake of saturated fats, increase in the intake of fruits, vegetables, whole grains, and oil, either through listening to a doctor’s advice or joining the forums, accompanied with regular exercise can assist in managing cholesterol levels. Sometimes it may call for a dose of some medications like statins to lower the LDL cholesterol with a view to reducing the prospects of developing carotid artery diseases, which may necessitate interventions such as carotid endarterectomy in severe cases.
3. Smoking
Statistical evidence exists chronicling a direct correlation between carotid artery disease and smoking hence creating a sobering revelation implicating smoking as a main cause of carotid artery disease. Tobacco smoke contains chemicals that are detrimental to human’s health; it causes the linings of the arteries to thicken, which hinders their elasticity, creates crevices where plaque can accumulate.
Smoking also minishes the oxygen supply in the blood vessels, raises blood pressure and rate of heartbeat, which are all factors that increase the vulnerability to formation of atherosclerosis as well as the progression to conditions that might necessitate interventions like carotid endarterectomy. Tobacco smoking is one more variable which enhances the CA and other cardiovascular diseases risk, That is why, smoking cessation among underage individuals is one of the most powerful protective factors. Quitting smoking and avoiding cigarettes include using support programs, drugs, and consultation.
4. Diabetes
Diabetes is a disease which develops when the body cannot work efficiently with glucose and therefore has high concentrations of glucose in the blood stream. High levels of glucose in the bloodstream affect the proper functioning of blood vessels, and this is also a reason for plaque formation in arteries.
Carotid artery disease will manifest in any patient with diabetes type 1 or diabetes type 2. Normal meal plans, exercise, blood glucose control and correct medication dosage reduces possibilities of Cardiovascular diseases among diabetic persons. Some of the complications associated with diabetes include carotid artery disease that may require interventions such as carotid endarterectomy.
5. Obesity
Specifically, abdominal obesity has been associated with the development of atherosclerosis. It also complicates such diseases as hypertension, elevated cholesterol levels, and diabetes. These conditions contribute to the development of carotid artery diseases. Occasionally, these diseases require procedures like carotid endarterectomy.
Healthy eating habits can achieve this by ensuring that the portion sizes contain foods with lower energy density. Exercise also plays another important role in the attainment of this goal. In total, weight loss is beneficial to the heart even if the number of total arteries is not significantly diminished; weight loss can also help to avoid carotid artery diseases.
6. Sedentary Lifestyle
The medical science has suggested that one of the causes of carotid artery disease is inactivity for a certain period of time. The recommended aerobic exercise assists people to keep their heart healthy without the formation of plaques in blood vessels. It also helps in the control of blood pressure, cholesterol and body weight.
To have a better cardiovascular profile, one must engage in at least 150 minutes of moderate-intensity activities. Such activities may be brisk walking, swimming, or cycling during the week depending on one’s schedule. Therefore, researchers tested the effects of moderate physical activity (PA) on weight status among adults in daily life.
7. Unhealthy Diet
Other risk factors for CAD include eating foods high in saturated fats, trans fats, cholesterol, and sodium. The above mentioned dietary factors thus contribute a lot in the development of this coronary artery disease. These dietary components can increase cholesterol in the circulating blood. It also raises blood pressure, and both factors can lead to the development of plaque on the inner walls of the arteries.
The dietary recommendations include; taking fruits, vegetables, whole grains, lean foods and foods low in saturated fats. These choices assist in decrease of the probability of the formation of atherosclerosis and thus maintaining cardiovascular health. Consuming less or avoiding, the processed foods as well as other foods with high sugar content is also good for the heart.
8. Family History
Carotid artery disease is often hereditary. Active contact with family members who have been affected by the disease can influence it. Some individuals have a genetic predisposition to cholesterol and blood pressure issues linked to cardiovascular diseases (CVDs). Those with affected relatives should prioritize their cardiovascular health through regular check-ups and preventive measures.
This means that anyone predisposed to the sickness has a higher chance of developing carotid artery disease. Therefore, annual check-ups should be a priority. Additionally, maintaining a healthy diet, regular exercise, and taking necessary action if symptoms appear are crucial steps for managing health effectively.
Diagnosis of Carotid Artery Disease
Diagnosing Carotid Artery Disease involves outlining the medical history of a patient and examining their general body systems. Doctors then conduct check-ups to determine the presence of plaque within the carotid arteries. Hence, there should be advancements in diagnosing it in its initial stages. Steps should be taken to minimize the chances of strokes.
1. Medical History and Physical Examination
The first medical step that the doctor takes in diagnosing patients with carotid artery disease is questioning the patient. The doctor then performs a physical assessment of the patient. During this consultation, the doctor engages in a discussion to understand the patient’s complaints. The doctor also investigates whether the patient has developed socially undesirable habits such as smoking and careless eating habits. Additionally, the doctor may inquire about the patient’s family history of diseases like cancer.
During the physical examination, the doctor listens for a sound in the carotid arteries called a bruit. The sound suggests possible stenosis, where narrowing of the arteries may cause turbulent blood flow. The presence of a bruit prompts further assessment to evaluate the severity of the condition. The first test assists the Doctor in an assessment as to whether the patient requires any other tests.
2. Carotid Ultrasound
Carotid Doppler scan, abbreviated as carotid duplex ultrasonography, is a noninvasive procedure. It locates and images the carotid arteries in real-time by emitting sound waves that bounce off the blood vessel walls as echoes. This technique provides detailed images without the need for invasive measures. This test also identifies the presence of plaque, its location, and the extent to which it has progressed deep into the arteries. It provides valuable information about the severity and distribution of plaque buildup within the arteries. They also enter the arterial blood vessels at certain rates to contribute to the measure of constriction.
Doctors commonly conduct carotid ultrasound tests as an initial examination for carotid artery diseases. This test is non-invasive and does not penetrate the skin or mucous membranes. It offers valuable information about the condition of the arteries and is considered safe and informative.
3. Computed Tomography Angiography (CTA)
X-ray combined with a certain dye is used to take pictures of the carotid arteries. A healthcare provider injects dye into a vein to visualize the arteries using fluoroscopy. X-ray pictures are then taken to observe and assess the arteries’ condition. Despite its limitations in describing plaque composition and location, CTA accurately assesses the degree of stenosis. It is valuable for providing detailed insights into arterial narrowing.
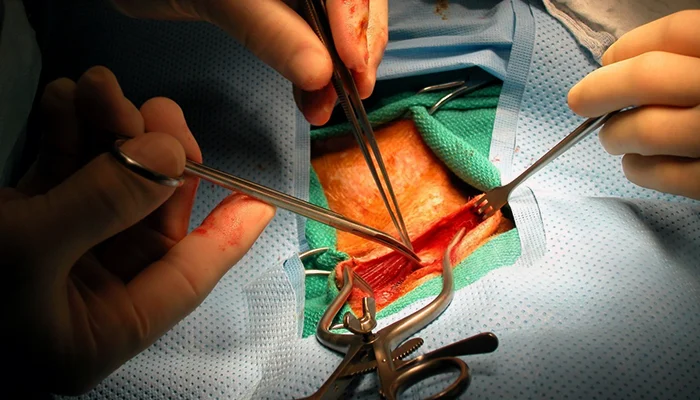
This imaging technique is highly relevant for surgeries like carotid endarterectomy. It helps visualize the condition of arteries through detailed images, aiding in surgical planning and execution.
4. Magnetic Resonance Angiography (MRA)
MRA refers to Magnetic Resonance Angiography and it is biomatically similar to an MRI scan though it is only performed on blood vessels using the power of magnetic fields and radio waves in order to enhance vessels outlines. It has been suggested that like CTA MRA can be able to give correct information as regard to the location of carotid arteries and the degree of stenosis.
It is carried on patients that cannot be subjected to CTA, it can be as a result of an unfavourable effect to the dye used in CTA or allergy to the dye. The distinguishing advantage of this modality is its ability to present images, for the purpose of assessment, examination or management of a disease. It is a helpful modality that offers detailed pictures in order to help in diagnosis or guide treatment.
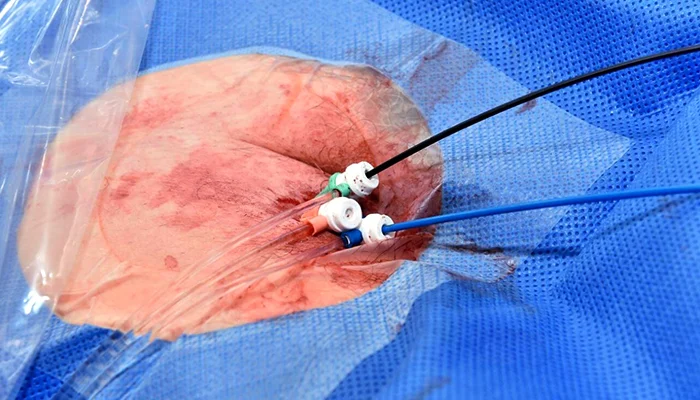
5. Carotid Angiography
Carotid angiography or cerebral angiography displays the carotid arteries through direct visualization. It is more invasive than other procedures such as Doppler sonography or magnetic resonance angiography. The process involves the use of a catheter to be placed in a blood vessel with the aim of filling it with contrast material for imaging. This procedure entails passing a catheter through a blood vein in the arm or leg. The medical professional moves the catheter in the direction of the carotid artery for imaging. It allows for direct visualization of the arteries using contrast dye and X-ray imaging techniques.
Contrast dye is administered through the catheter for this procedure, and X-ray imaging is used. Carotid angiography is less common and physicians typically perform it when other imaging studies fail to provide sufficient information. Some surgeons also use it for better analysis and preoperative planning of carotid surgeries. The procedure includes the use of contrast dye and X-ray imaging of the arteries in order to capture minute details. It is adopted by the doctors so that they can be in a position to assess the arteries and come up with the right treatment.
6. Blood Tests
Doctors sometimes recommend lifestyle modifications if a person is at risk of developing carotid artery disease. These modifications include changes in diet and exercise routines. Blood tests monitor cholesterol and diabetes levels to assess the risk. These tests can reveal other conditions such as diabetes that must be controlled to minimize the formation of atherosclerosis and other related complications.
They can perform basic tests such as blood sugar and cholesterol levels. These tests help identify complications of the heart and guide specific treatment plans. Regular testing is crucial for managing heart health and preventing complications.
7. Electrocardiogram (ECG)
An electrocardiogram (ECG) records the electrical signals of the heart to rate its pacing and depolarization. While ECG does not diagnose carotid artery disease, it diagnoses other cardiovascular diseases including heart disease and arrhythmias related to carotid artery diseases that needs management.
It is necessary for the caregivers as well in order to carry out the exposures concerning his/ her credentials and the status of the heart as well as touch with the psychosocial prognosis and other interrelated domains of cardiovascular sickness control.
Conclusion
Of all the examined types of cardiovascular disease, it is known that carotid artery condition itself poses an independent risk factor for stroke incidents, primarily caused by atherosclerosis. These are some of the general causes of this heart condition including high blood pressure, high cholesterol, smoking, diabetes, obesity, spotless phenotype, no exercise, no balanced diet and family history. Through clinical examination and the patient’s history and some other complementary tests like carotid ultrasound, CTA, MRA, carotid angiogram, blood examination and EGG should be used to diagnose the extent of carotid artery disorders in the early stages. By addressing risk factors and utilizing appropriate diagnostic methods, individuals can significantly reduce their risk of stroke and improve their overall cardiovascular health.