Peripheral vascular disease (PVD) is a disorder that affects the blood vessels located outside the heart and the brain, mainly in the arms and legs. These channels are essential for providing oxygen-rich blood to varied body parts and, consequently, help them maintain normal functioning. Narrowing or blocking of these blood vessels reduces blood flow, leading to pain, numbness, or weakness in the affected limbs. This article will discuss the causes of PVD and how doctors diagnose this condition.
Causes of Peripheral Vascular Disease

Many factors contribute to the pace of peripheral vascular disease. These causes should be understood correctly, as they are indispensable for prevention and treatment. Here are some of the primary factors:
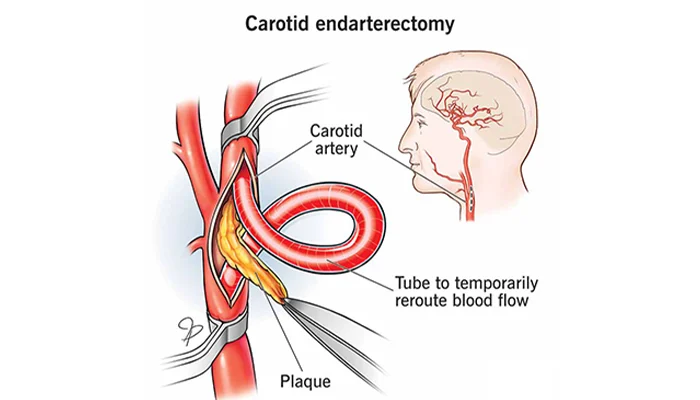
1. Atherosclerosis
Among other things, atherosclerosis, which is the most common cause of peripheral vascular disease, is a significant factor that leads to this. It is the outcome of fat-rich substances called plaque that clog up the artery walls. Because of this plague deposit, these arteries will tightly constrict. Veins have reduced blood flow, causing less oxygen and fewer nutrients to reach the tissues behind the clot. With time, plaque might get harder, making narrowing arteries and damaging current efficiency in expansion and contraction even worse.
2. Smoking
Smoking is one of the main risk factors for the disease called “peripheral vascular disease” The smoke components are detrimental to the inner layer of the veins, and so they are more vulnerable to the accumulation of plaque. This damage not only helps plaque build-up formation but strain inflammation and clotting formation as well. Not only does smoking cause blood pressure and cholesterol levels to increase, the occurrence of various vascular diseases is also convincing.
3. Diabetes
Diabetes can damage the vessels that transfer blood and nerves that could have peripheral vascular disease. Impaired levels of blood sugar due to diabetes cause inflammation and damage the inner wall, leading to its veins being vulnerable to atherosclerosis. This situation leads to the formation of fat deposits that clog up the arteries, limiting blood flow. More or less, diabetes contributes to the development of circulatory problems in the eyes, kidneys, and nerves (this includes circulation of the arms and legs).
4. High Blood Pressure
Hypertension, which is a synonym for high blood pressure, is a powerful factor that makes your blood vessels quite unstable. This pressure can be the cause of damage to the walls of your blood vessels, which get thinner and weaker with time. Eventually, the progression of this narrowing can further result to the occurrence of peripheral vascular disease where your arteries in the hands and feet become vascularized and blood flow is restricted.
5. High Cholesterol
The artery sclerosis or peripheral arterial disease can develop due to the mechanisms of an artery clogging by cholesterol. With the atherosclerosis of arteries as its partner in crime, peripheral vascular disease becomes more evident in the long run. The LDL cholesterol, the “bad” cholesterol which is usually to blame for the appearance of this plaque when it accumulates.
6. Obesity
The overweight or obesity is the leading factor in lymphatic disease. The long term effects of texting while driving could be the development of high blood pressure and other cardiovascular problems. These problems can appear gradually, making them additionally dangerous. As this happens, your peripheral vascular system becomes at risk (blood vessels in your arms and legs narrow and restrict blood flow).
7. Inactive Lifestyle
Non-participation in physical activities can be one of the causes of peripheral vascular disease. For example, regularly practicing activities like walking or biking helps ensure uninterrupted blood flow, avoiding clogging in the arteries. For this reason, you must stay active to prove to yourself that your heart is in a good state and less likely to suffer from peripheral vascular disease.
8. Age and Genetics
As we grow up, our blood vessels become increasingly worn, losing flexibility and becoming easily damaged. Apart from all this, the natural aging process can increase the dangers of peripheral vascular diseases because it worsens the ability of arteries to dilate. Genes also participate in the process of the development of the diseases. Therefore if members your family has PVD, you will have a reason to worry about it too. This indicates that the person concerned who has developed symptoms of peripheral artery disease with a positive history of ageing is indeed prone to the disease.
Diagnosis of Peripheral Vascular Disease
The initial stages of PVD diagnostic process involve asking a patient health history, conducting a clinical examination, and applying a special test. Here are the common diagnostic methods used for detecting and confirming PVD:
1. Medical History and Physical Examination

Your first doctor’s visit at the very onset will be to carry out any investigations that might be needed, as well as a holistic lab and physical examination. While doing this procedure, they will ask you about the symptoms that you are having, like leg pain, numbness or wounds, and they will also get information about your general health and lifestyle. During the observation of your legs, the physical exam will also include checking for certain signs that may indicate PVD, such as weak pulses, cold skin, and non-healing wounds.
This first examination gives information about your condition and risk factors. The data will help the doctor select the best way to deal with the possible presence of PVD. It is you, the doctor who will have to carry out the assessment and make any decision on whether to carry out any additional diagnostic procedures in the light of the review of the medical history and the results of the physical examination.
2. Ankle-Brachial Index (ABI)
ABI test is a practical procedure of arterial blood pressure between the arms and ankles to determine the blood vessels’ functionality. Place blood pressure cuffs on your upper arms and ankles, the two locations of the device. Additionally, use a Doppler ultrasound probe to measure blood pressure in all three positions. Calculate the ratio of ankle pressure to arm pressure. A lower ABI ratio indicates poor blood flow to your legs, suggesting the possibility of PVD.
ABI is a straightforward and result-oriented technique designed to screen for peripheral arterial disease of the legs. It is useful to spot possible obstructions or narrowing of the arteries and thus get information about the degree of PVD.
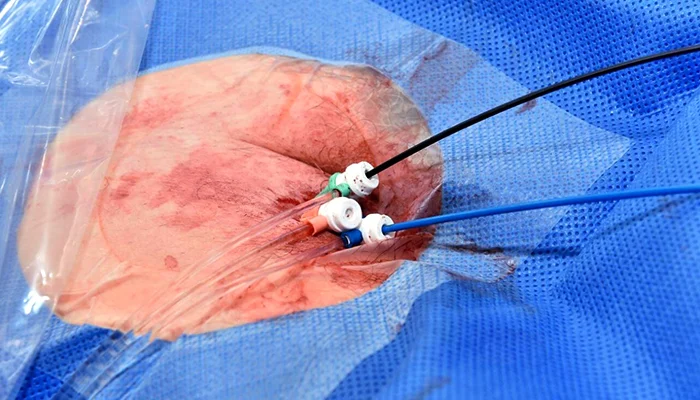
3. Doppler Ultrasound

Doppler sonography as a non-invasive imaging method provides images of blood vessels based on the ultrasound wave as information carriers. A doctor will apply a gel onto the skin area above the blood vessels and then use a transportable device called a transducer; this tool utilizes immediate frequencies to transmit and receive sounds. It uses the motion of sound waves as a tool for observation. These images can serve as references in case of blood flow anomalies.
Doppler sonography provides real-time pictures of the blood flow in the arteries and veins. This allows your doctor to discover blockages, narrowing, or other abnormalities that may indicate PVD. Also, It is typically used as a primary diagnostic tool, but it can also lead to other facilities and treatment options.
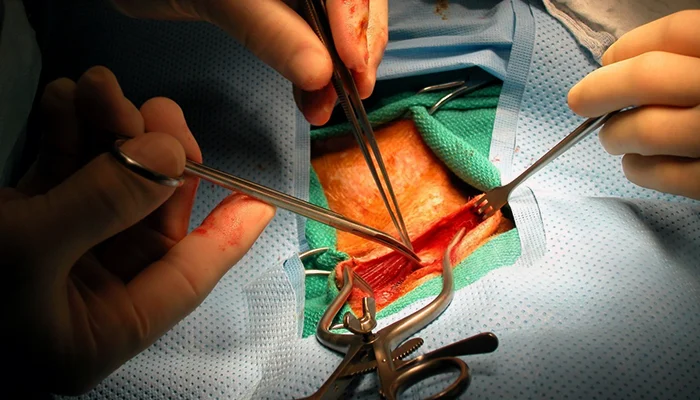
4. Angiography
Angiography injects a dye contrast into the blood vessels for an X-ray examination, utilizing a developed non-invasive approach. Subsequently, after injecting the dye, the doctor waits for the screening pictures, which are used to evaluate the anatomy and condition of the blood vessels.
Angiography involves creating structural images of the vessel system. These images pinpoint the location and amount of the narrowing or blockage. This method is usually employed to design actions like angioplasty or stenting to advance blood circulation in patients with PVD.
5. CT Angiography or Magnetic Resonance Angiography (MRA)
The latest, CT angiography and MRA imaging technology is used when doctors need to see the whole blood vessel structure. CT angiography uses X-rays and a contrast dye to make pictures of your arteries and veins, while the MRA do not use X-rays or contrast dye and the images are produced by powerful magnets and radio waves.
It helps professionals understand the vascular architecture accompanied by blocks and anomalies, which play a key role in developing PVD. These imaging tests are particularly useful for planning surgical interventions or monitoring disease progression.
6. Blood Tests
Blood tests might be carried out to help evaluate cholesterol levels among other factors. These factors may contribute to both PVD and vitreoretinal diseases, such as blood sugar levels and markers of inflammation. High levels of cholesterol in your body can increase the risk of developing PVD and other cardiovascular conditions. Elevated blood sugar levels can also contribute to this heightened risk. These blood tests are studied by the doctor to help achieve the diagnosis of your disease. They also assist in properly managing the condition.
Blood tests are an essential diagnostic tool. They visualize the overall cardiovascular system’s condition and may reveal potential risk factors related to PVD. By continuously monitoring your cholesterol levels, blood sugar levels, and other indicators, your doctor can gather valuable information. This allows them to compile a customized treatment plan aimed at reducing the risk of complications and improving your overall health.
Taking Control of Your Vascular Health
Peripheral vascular disease (PVD) is a common condition. If not treated in time, it can sometimes be severe and significantly affect your quality of life. Understanding the causes and risk factors that contribute to PVD is essential. It will help you take preventive or management measures for this condition. If you are experiencing cavitations, leg pain, numbness, or if your wound is not healing, it is important to seek medical care promptly. Ask for a medical consultation for diagnosis and treatment. Detecting the problem early and taking action increases the likelihood of maintaining good vascular health. This can lead to enjoying better overall well-being.